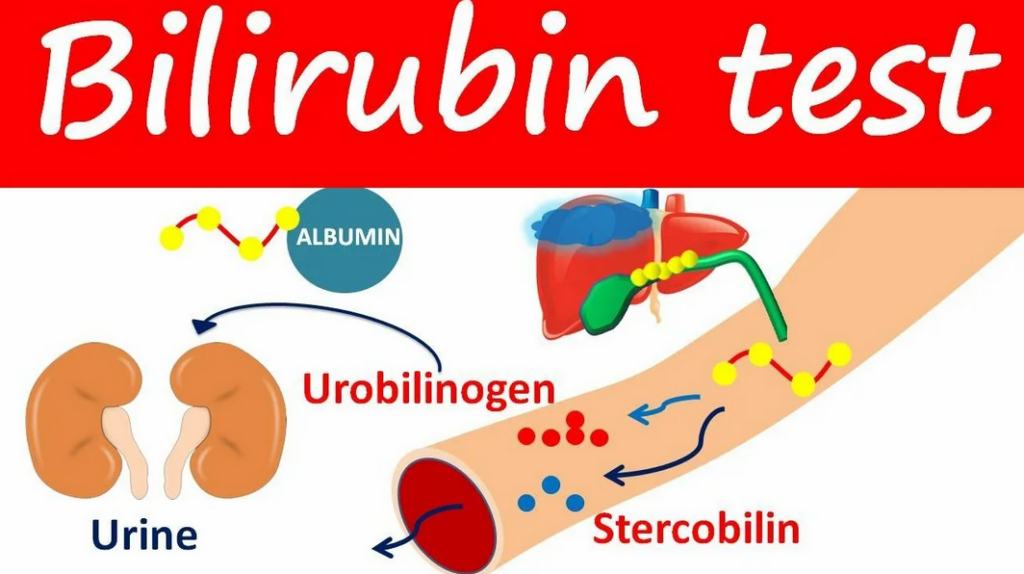
Bilirubin is a bile pigment formed during the breakdown of hemoglobin from old red blood cells. It exists as indirect (unconjugated) and direct (conjugated) bilirubin, and their sum is the total bilirubin.
| Parameter | Characteristics |
|---|---|
| Indirect Bilirubin | Insoluble in water, toxic. Transported to the liver bound to albuminOne of the main proteins of the human body, responsible for maintaining normal blood composition and transporting various substances throughout the body. It also serves as a reserve source of amino acids. Albumins perform two very important functions: managing the distribution of water within the body, helping the blood transport vitamins, minerals, and medications. They are responsible for water exchange — they help retain it in the vessels and prevent it from excessively moving into the tissues (thus preventing the development of edema). Albumins influence the formation of tissue fluid, urine, and lymph, and also control the process of water absorption from the intestines.. |
| Direct Bilirubin | Formed in the liver after conjugation with glucuronic acid. Excreted in bile. |
| Total Bilirubin | The sum of direct and indirect bilirubin. |
| Type of Bilirubin | Normal Range (Adults) |
|---|---|
| Total | 3.4–20.5 µmol/L |
| Direct | 0–5.1 µmol/L (≤25% of total) |
| Indirect | <19 µmol/L |
Note: In newborns, bilirubin can temporarily rise to 200–250 µmol/L (physiological jaundice).
Causes:
Symptoms:
Causes:
Symptoms:
Rare and usually not clinically significant.
Possible causes:
Symptoms:
Absent, but may correlate with a low level of antioxidant protection.
| Ratio | Diagnosis |
|---|---|
| Indirect ↑, Direct normal | Hemolysis, Gilbert’s syndrome |
| Direct ↑, Indirect normal | Hepatitis, gallstone disease |
| Both ↑ | Severe liver damage |
Important: Jaundice is not always liver disease! Clarify the type of bilirubin for accurate diagnosis.