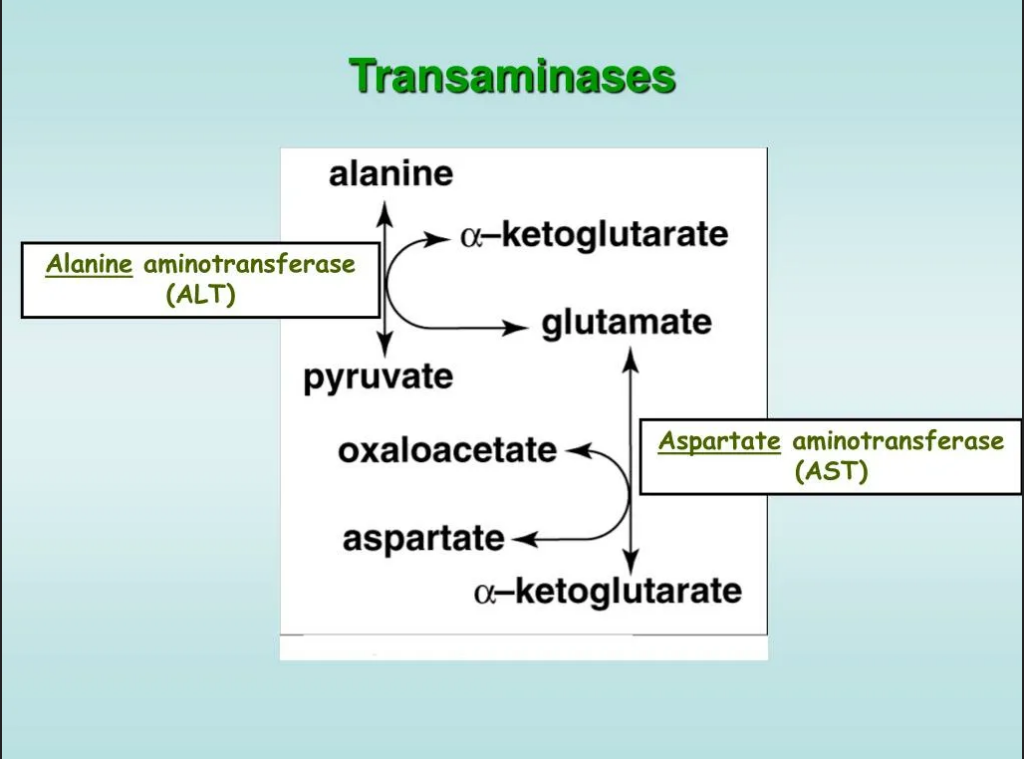
ALT is an enzymeEnzymes are proteins that accelerate chemical reactions in the body. They ensure the occurrence of metabolic processes such as food digestion, energy release, cell formation, and many others. found primarily in liver cells, but also in smaller amounts in the kidneys, heart, and muscles. When these organs are damaged, ALT is released into the bloodstream, making it an important marker of liver disease.
| Category | Reference Values (U/L) |
|---|---|
| Men | 10–40 (up to 50 in some laboratories) |
| Women | 7–35 |
| Children | Up to 30–45 (age-dependent) |
Note:
Reasons:
Symptoms of excess (in liver diseases):
How dangerous is it?
ALT deficiency is an extremely rare condition, as the enzyme is normally present in the blood in small amounts.
Possible reasons:
Symptoms of deficiency:
How dangerous is it?
To clarify the diagnosis, prescribe:
For prevention purposes: